Introduction
Hepatitis C virus (HCV) remains a significant global health concern, with an estimated 71 million individuals chronically infected. This blog post delves into the epidemiology and public health aspects of HCV, exploring its global burden, transmission routes, and current prevention strategies.
Global Burden of HCV
HCV distribution exhibits significant geographical heterogeneity. The World Health Organization (WHO) estimates the highest prevalence in the Eastern Mediterranean and African regions, exceeding 8% in some countries. These regions also carry a disproportionate burden of disease complications like cirrhosis and hepatocellular carcinoma (HCC). Factors contributing to this disparity include unsafe healthcare practices, limited access to clean water and sanitation, and high rates of injection drug use.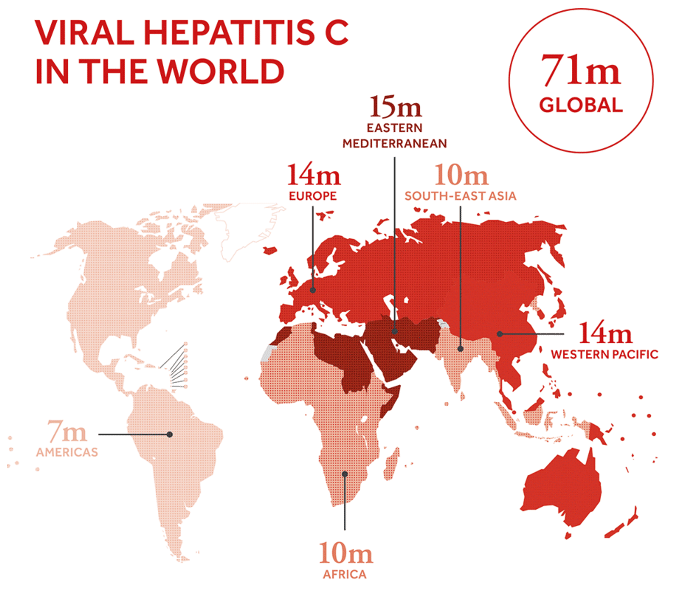
Transmission Routes of HCV
HCV is primarily transmitted through contact with infected blood. Sharing needles and syringes during injection drug use represents a major risk factor, particularly in resource-limited settings. Unsafe healthcare practices like inadequately sterilized medical equipment can also facilitate transmission. Vertical transmission from mother to child can occur, but the risk is relatively low (1-5%). Sexual transmission of HCV is possible but less efficient, with a higher risk associated with co-infection with HIV or other sexually transmitted infections.
Current Prevention Strategies
Harm Reduction Programs: These programs provide injection drug users with sterile needles and syringes, education on safe injection practices, and access to addiction treatment. Studies have shown that harm reduction programs significantly reduce HCV transmission rates among this population.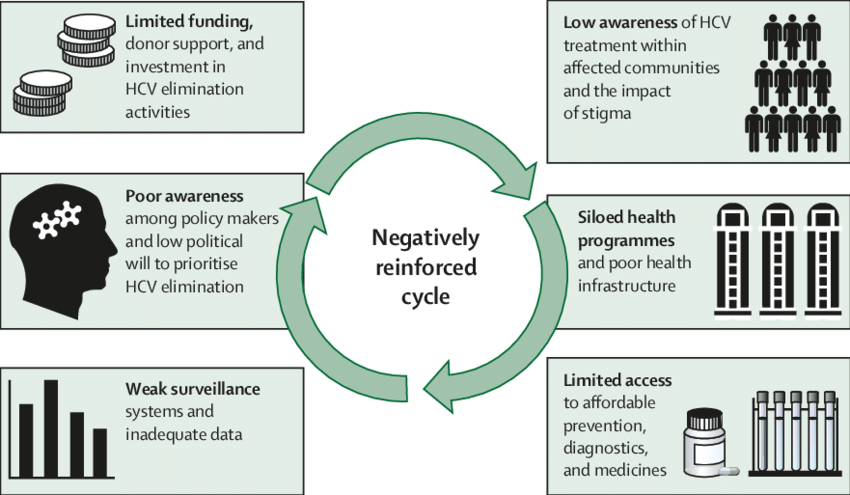
Vaccination:
Currently, no commercially available vaccine exists for HCV. However, research and development efforts are ongoing, focusing on identifying immunogenic viral targets and designing effective vaccine platforms.
Blood Screening and Safe Healthcare Practices:
Universal blood screening for HCV in blood donations significantly reduces the risk of transfusion-associated transmission. Implementation of stringent infection control practices in healthcare settings is crucial for preventing nosocomial transmission.
Beyond the Lab: Fast and Easy Detection of HCV with the Anti-HCV Card ICT
The Anti-HCV Card Immunochromatographic assay (ICT) serves as a rapid point-of-care (POC) diagnostic tool for the initial screening of Hepatitis C virus (HCV) infection. This user-friendly test relies on immunochromatography, a technique that utilizes specific antibodies immobilized on a membrane to detect the presence of HCV antibodies in a patient's blood, serum, or plasma sample. During the test, the sample migrates along the membrane, encountering immobilized HCV antigens. If anti-HCV antibodies for examle those offered bu Gentaur are present in the sample, they bind to the antigens. A secondary antibody linked to a visible marker (often a colored dye) then binds to the antigen-antibody complex, generating a visually detectable line on the test cassette. A positive result on the Anti-HCV Card ICT indicates potential past or present exposure to HCV. However, it's crucial to note that a positive result from this rapid test requires confirmatory testing using a more sensitive method like HCV RNA detection to definitively diagnose active infection. 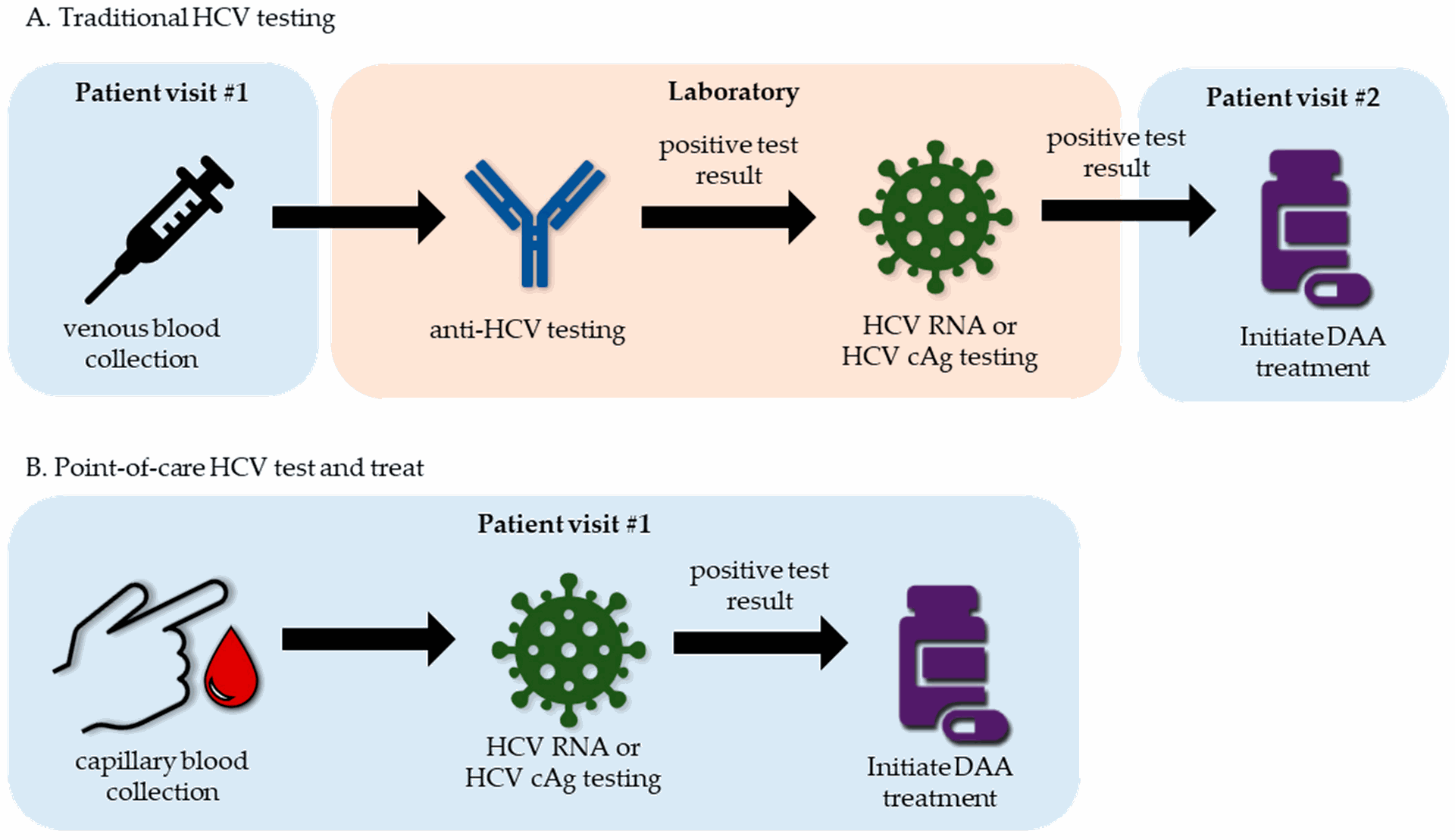
Conclusion
Despite the availability of highly effective treatments, HCV remains a significant public health burden. Implementing and scaling up existing prevention strategies, particularly harm reduction programs, alongside research and development of an HCV vaccine, are crucial steps towards achieving global HCV elimination.